- Visibility 123 Views
- Downloads 5 Downloads
- DOI 10.18231/j.aprd.2025.004
-
CrossMark
- Citation
Dr. Per-Ingvar Brånemark: A pioneer in osseointegration and modern dental implants
Introduction
Early life and education
Per-Ingvar Brånemark, born on May 3, 1929, in Karlshamn, Sweden, was a distinguished physician and anatomist. He earned his medical degree from the University of Lund in 1956 and completed his PhD in 1959. Born as Per Ingvar Persson, he initially published his early work under this name. Later, he adopted the surname 'Brånemark’, which translates to "one who breaks the ground." This name symbolized his groundbreaking achievements in medicine and science. Known as the father of modern dental implantology, Brånemark revolutionized dental implants and prosthetics through his pioneering research in osseointegration, transforming the quality of life for countless individuals.[1], [2] ([Figure 1]).
The accidental discovery of osseointegration
Brånemark's PhD research focused on "Vital Microscopy of Bone Marrow," utilizing an optical device encased in a titanium mesh to examine blood flow in rabbit tibia bone. He observed that, over time the titanium had fused so securely with the bone that it could not be removed without fracturing. After consulting with a university linguist, Brånemark later coined the term "osseointegration" to describe the secure attachment of titanium to bone tissue. [3] He chose to investigate this occurrence independently, despite the fact that it was not the intended focus of the study. [4], [5] Per-Ingvar's extensively cited thesis on microcirculation in bone, fetched him a post of associate professor and ultimately, Professor at the Department of Anatomy in Gothenburg the following years. He established his own laboratory and engaged in collaborative research with others and continued his study on microcirculation in animals and eventually expanded the investigations to include humans. [6]
Challenges in proving osseointegration
Brånemark was convinced beyond doubt that his experimental titanium mesh had anchored in bone tissue in rabbits. [7] This ran counter to the ideas of the time, which held that metal could never be directly anchored to bone, as it will produce foreign body reaction leading to its rejection. [8], [9] Unfortunately, his attempts to prove his theory of bony union relied on low-power images or specimens that had been decalcified, necessitating the removal of the implant before bone could be sectioned. In the process of removing the implant, the interfacial soft tissues were also inevitably removed, causing others to doubt the bony anchorage. Later on, Donath's discovery of the cutting and grinding approach allowed for the examination of entire bone-to-metal interface.[10] Brånemark's theories on integration between titanium and bone were confirmed at the light microscope resolution. Before the establishment of bony anchorage, he struggled to secure funding for his investigations.
In 1965, Brånemark implanted optical titanium chamber in the left upper arm of twenty staff volunteers working in his lab to conduct crucial microscopic investigations on human microcirculation and intravascular behavior of blood cells at high resolution. Fortunately, the titanium chambers showed no unfavorable inflammatory reactions and his experiment validated the suitability of titanium for use in the human body. Because he believed that the implants' bone anchorage would enable them to work successfully in a clinical context, he applied the notion of osseointegration to dental implants in the edentulous jaw without waiting for the resolution of academic disagreement. [11]
Discussion
Development of modern dental implantology
In 1965, Brånemark placed the titanium dental implants in the first human patient, Gösta Larsson, who had severe jaw deformities, including cleft palate and edentulous lower arch. These implants remained functional for the rest of the patient’s life, demonstrating their long-term success. This marked a turning point in dentistry and Brånemark's pioneering work laid the foundation for modern dental implants, greatly enhancing patients' quality of life by offering a reliable solution for missing teeth. Following this, Brånemark’s journey continued relentlessly, with his vision captured in a poignant quote: "No one should die with their teeth sitting in a glass of water." This statement underscores his unwavering dedication to restoring dignity and improving the lives of those who had lost their teeth.
Overcoming skepticism in implantology
At this time, academic dentistry did not support the use of oral implants, and Swedish dental professionals heavily criticized his clinical practices. It was not until 1977 that the issue began to be solved, following a largely favorable clinical report by several Swedish academicians on the success of dental implants. [12] After significant effort and evidence, Brånemark obtained the financial backing necessary to advance his research, ultimately leading to the development of widely recognized and adopted osseointegration procedures. His journey serves as a testament to the importance of perseverance and resilience in scientific exploration.[12]
Pioneering osseointegration research
Brånemark originally defined osseointegration as a direct structural and functional connection between ordered living bone and the surface of a load-carrying implant. [13] He later expanded on this concept, and stated that “osseointegration in theory and practice is defined as continuing structural and functional coexistence, possibly in a symbiotic manner, between differentiated, adequately remodeled, biologic tissues and strictly defined and controlled synthetic components, providing lasting, specific clinical functions without initiating rejection mechanisms”. His definition highlighted a continuing coexistence between the implant and surrounding tissues, emphasizing the importance of biocompatibility and the absence of immune rejection. Osseointegration was explained by Brånemark through three distinct stages. [5], [14]
The initial implantation phase
Immediately following implant placement, primary stability is achieved through the physical engagement of the implant threads with the surrounding bone. This mechanical interlocking ensures that the implant remains securely anchored within the bone, providing an essential foundation for the subsequent healing process and osseointegration. To optimize primary stability, Brånemark emphasized the importance of minimizing trauma to the surrounding bone and soft tissues, removing only the necessary amount of bone, and preserving the natural topography of the implant site. The size of the prepared osteotomy will be a slight mismatch with the size of the implant. This allows hematoma to form within the socket, filling the space between the implant threads and the surrounding bone. The bone adjacent to the implant experiences unavoidable thermal and mechanical trauma during the drilling and insertion process. Beyond this zone of injury lies intact, undisturbed original bone that remains structurally sound and in proximity to the implanted fixture, providing a foundation for the subsequent healing and osseointegration process. ([Figure 2]A)
The unloaded healing phase
The hematoma within the implant site undergoes a transformation into new bone through the process of callus formation. This gradual conversion aids in the integration of the implant with the surrounding bone. Simultaneously, healing of the traumatized bone is facilitated by neovascularization, and through cycles of de and remineralization. ([Figure 2]B)
Post healing phase
Vital bone tissue directly contacts the surface of the implant fixture, with no intervening connective tissue. The bone in the surrounding zone remodels in response to the masticatory forces applied during function. ([Figure 2]C)
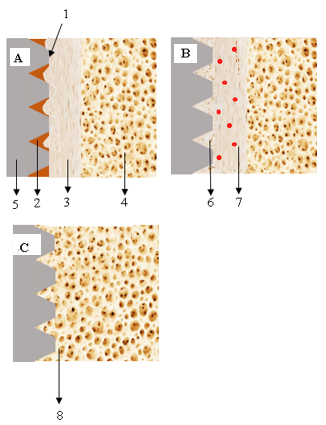
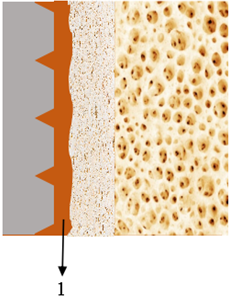
In unsuccessful implants, nonmineralized connective tissue can develop in the border zone around the implant ([Figure 3] ). This outcome is often triggered by factors such as excessive trauma during preparation, infection, premature loading during the healing period before sufficient mineralization and organization of hard tissue, or excessive loading at any point, even years after initial integration. Branemark advocated delayed loading and cautioned against premature or excessive loading of the implant during the healing process. He recommended waiting until sufficient mineralization and organization of the bone tissue had occurred to avoid implant failure. While Brånemark initially focused on a delayed loading approach, he did not completely dismiss the idea of immediate loading. Over time, his research and clinical practices evolved, paving the way for immediate loading protocols in certain cases.
Collaboration and global impact
Recognizing the transformative potential of osseointegration, Brånemark shifted his focus to exploring other practical applications of this discovery. Bofors, now Nobel Biocare, played a pivotal role in globalizing his innovation by commercializing the Brånemark Implant System and its associated treatment protocol.
Other applications of osseointegration in dentistry
Ad modum protocol
Ad modum, the original Brånemark protocol for dental implant treatment, called for an initial 3–6 months healing period during which the implants were submerged in bone tissue to induce osseointegration before loading.[15] This concept focused on restoring the edentulous maxillary or mandibular arches by employing 4 or 6 commercially pure titanium screw-shaped implants in a two-stage procedure. [16] This research provided vital insights into an innovative method for treating patients with completely edentulous upper or lower jaw.
Novum protocol
When the Brånemark system was first introduced, it was envisioned as a two-step procedure that would enable bone remodelling before functional load was applied. In case of mandibular bone, the recommended healing time was between three and four months. On the other hand, the healing period for the maxilla, which is more cancellous, was proposed to be between five and six months. [15] In order to reduce the healing time, clinical visits and treatment cost, Brånemark and colleagues proposed a new protocol for edentulous mandible rehabilitation, known as Brånemark Novum, in 1996. [15] By combining one-stage surgery with quick loading implant principles, the Novum protocol (Nobel Biocare AB) streamlines the Brånemark classic protocol, enabling edentulous mandible rehabilitation on the same day of implant surgery. He suggested that all surgical and prosthetic treatments be completed in 6–8 hours. [17], [18] In this protocol, drilling templates were used to accurately place three titanium implants in the mandibular region (between the mental foramina). Right after insertion, these implants were firmly splinted using a pre-fabricated titanium bar. By securing the bar with titanium screws to the transmucosal implant, rotational forces were effectively prevented from approaching the bone-implant interface. [15] A prefabricated titanium prosthetic bar was then precisely connected to the implant stabilizing bar. At a predetermined vertical dimension of occlusion, bite registration was carried out. [19] On the day of implant surgery, a final implant-supported fixed prosthesis was made and fixed to the prosthetic bar, giving the patient permanent restoration. [15]
Expanding applications of osseointegration
Beyond dental applications, Brånemark's research extended to other medical fields. He explored osseointegration to anchor limb prosthetics directly to the skeleton, providing amputees with more stable and functional artificial limbs. This method called "osseointegrated prosthetics," has changed the lives of many people who used to have trouble with regular socket prosthetics. By connecting the prosthesis right to the bone, these new prosthetics are more stable, help people move better, and feel more natural.
Bone anchored hearing aids (BAHA)
Air conduction hearing aids were used earlier to treat patients with hearing impairment. However, these devices were ineffective for patients who had conductive hearing loss where the ear canal was affected due to congenital auditory atresia, recurrent otorrhea, or disorders of the ossicles. These patients needed to wear a headband of metal springs that had a vibrating device which applied pressure on the soft tissues of the skull, leading to pain and ulcerations. Brånemark collaborated with otolaryngologists at Sahlgrenska University Hospital and experts from Chalmers University of Technology in Gothenburg, Sweden and proposed placing a titanium implant within the mastoid process of the temporal bone behind the ear in such patients. After achieving osseointegration, an impedance-matched transducer capable of generating vibrations was attached to the implant, enabling direct transmission of these vibrations to the brain. [20] Even today, this innovation, known as the bone-anchored hearing aid (BAHA), is used in cases where the outer ear canal and middle ear ossicles are compromised, but the inner ear remains functional. [12]
The Brånemark system was the first extraoral implant system to be employed. Currently, a large number of patients around the globe have seen positive outcomes from the utilization of BAHA, employing the identical osseointegrated titanium screws in lengths of 3, 4, and 5.5 mm. with a flange that was developed by Brånemark and Kuikka in 1977. These implants came with a flange to avoid intracranial dislocation through trauma. The Brånemark system is still available for purchase from Cochlear Company, marketed as Vistafix. [3], [20], [21]
At the Department of Otolaryngology in Sweden, he met patients who, due to cancer surgery, trauma, or congenital abnormality, suffered from facial deformity and, these patients faced substantial challenges due to their conditions, with many opting for social isolation, and some even avoiding going outdoors during daylight hours. [20], [22] Brånemark displayed a keen interest in these cases, particularly focusing on larger defects. He embraced a multidisciplinary approach, collaborating with experts in fields such as oral surgery, prosthodontics, anaplastology, and engineering. Using the same implants designed for BAHA, he secured silicone maxillofacial prostheses to these implants, creating what became known as implant-supported maxillofacial prostheses. [22]
Implant supported maxillofacial prosthesis
Since their introduction in 1977 for use with bone conduction hearing aids, percutaneous endosseous implants have remained an important constituent part of prosthetic rehabilitation of patients with maxillofacial abnormalities, especially when surgical reconstruction is not feasible. Prior to their advent, the only methods available for securing these prostheses involved the use of adhesives, anatomical undercuts in soft or hard tissues, or glasses. However, these methods have limitations, including issues with adhesives, such as discoloration of the prosthetic materials. Additionally, adhesives and solvents can lead to both mechanical and chemical irritation of the skin and mucosal surfaces. Endosseous implants provide an excellent solution to these challenges, offering superior stability to the craniofacial prosthesis and eliminating the need for adhesives. Additionally, they enhance the aesthetic profile by allowing for precise prosthetic margins, leading to improved patient acceptance and satisfaction. [12]
Zygomatic implants
Zygomatic implants, introduced by Brånemark, provide a viable solution for patients with severe maxillary bone deficiencies where conventional dental implants are not feasible. They are also indicated for patients who have experienced failures with traditional implants or grafts, for those seeking a graft free alternative, individuals with congenital conditions such as cleft palate leading to the absence of maxillary bone, and patients who have undergone maxillectomies due to tumors or other diseases. [23] In 1998, Brånemark published a clinical report on zygomatic implants, documenting a 10-year follow-up of 164 implants anchored in the zygomatic bone, with an impressive success rate of 97% for the involved implants. [24] The technique used in this study employed implants ranging from 35 to 55mm in length, that was placed in the zygomatic bone crossing through the sinus and splinted to 2 to 4 conventional implants in the anterior region.[15]
Legacy and honors
Dr. Brånemark, widely regarded as the father of dental implantology, has received extensive recognition for his contributions, earning numerous awards and honors, including more than 29 honorary doctorates from universities worldwide. He received prestigious awards such as the Swedish Medical Association's Söderberg Prize in 1992 and the European Inventor Award by the European Patent Office. His legacy continues through the institutions and organizations he founded, including the Brånemark Osseointegration Center (BOC) in Gothenburg, Sweden, a leading center for research and training. In 2012, he was awarded the lifetime achievement award by the Greater New York Academy of Prosthodontics (GNYAP). He was also honored with honorary membership to the American Dental Association (ADA), one of the few non-dentists to receive this recognition. [1]
Impact on patient care
The practical outputs of Brånemark's work include so much. Dental implants as an outcome of his discovery of osseointegration have become, through millions of procedures annually, today the gold standard for tooth replacement. These implants have several virtues above traditional dentures or bridges, which include aesthetics and function and patient comfort. As stated, dental implant patients can have better oral health and the ability to function while eating and speaking without causing any discomfort. [7]
Osseointegrated prosthetics are full of promise for amputees with higher mobility and much comfort over conventionally fitted prosthetics. This growth has been rewarding for military veterans as well as others who have suffered through traumatic loss of limb[s]. [8]
Research and future directions
The field of osseointegration continues to evolve, with ongoing research aimed at improving implant materials, techniques, and outcomes. Advances in biomaterials, surface treatments, and imaging technologies hold promise for further enhancing implant integration and longevity. Brånemark's initial discoveries have paved the way for interdisciplinary collaborations, pushing the boundaries of reconstructive surgery and rehabilitation. [9], [10]
Personal reflections and humanitarian efforts
Beyond his scientific achievements, Brånemark was known for his compassionate approach to patient care. He believed in listening to patients and understanding their needs and experiences, driving his desire to improve their quality of life through innovative medical solutions. His humanitarian efforts extended beyond his clinical practice, as he was committed to providing dental and orthopedic care to underserved populations worldwide. His work has had a lasting impact on the field of medicine and the lives of countless individuals, underscoring the importance of using scientific advancements for the betterment of society.
Conclusion
The contributions of Dr. Per-Ingvar Brånemark to medical science and patient care are monumental, and his discovery of osseointegration remains a cornerstone in modern dentistry and reconstructive medicine. His revolutionary application of titanium implants has transformed the treatment of edentulous patients into a functional, aesthetic, and long-lasting solution. Outside of dentistry, his innovations extended to bone-anchored hearing aids, implant-supported craniofacial prostheses, and osseointegrated limb prosthetics, improving the quality of life for countless individuals with unique medical challenges.
Brånemark's perseverance in overcoming initial skepticism and funding challenges underlines his unwavering commitment to advancing science and improving patient outcomes. His methodologies, such as the Brånemark Novum and zygomatic implant protocols, streamlined surgical procedures and reduced treatment times, making rehabilitation accessible and efficient.
Brånemark's legacy continues through continuous progress in implantology. His research inspired continuous innovation in biomaterials, surgical techniques, and patient care strategies. His humanitarian approach stressed that patients be treated with dignity and functionality restored to them; thus, science should serve humanity.
Dr. Brånemark’s life was not merely a milestone but a transformative force in healthcare. His contributions reshaped medical paradigms, leaving a lasting impact that continues to evolve over the years. As time passes, generations of physicians and patients around the world will continue to regard his work as an enduring source of inspiration.
Source of Funding
None.
Conflict of Interest
None.
References
- . American College of Prosthodontists. (2024). Branemark. 2024. [Google Scholar]
- B Per-Ingvar, GA Zarb, A Tomas, R Harvey. Tissue-Integrated Prostheses. Osseointegration in Clinical Dentistry. Plast Reconstr Surg 1986. [Google Scholar]
- R Brånemark, PI Brånemark, B Rydevik, RR Myers. Osseointegration in skeletal reconstruction and rehabilitation: a review. J Rehabil Res Dev 2001. [Google Scholar]
- T Albrektsson, G Zarb, P Worthington, AR Eriksson. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants 1986. [Google Scholar]
- PI Brånemark. Osseointegration and its experimental background. J Prosthet Dent 1983. [Google Scholar]
- G Zarb, U Lekholm, T Albrektsson. In memoriam: Per-Ingvar Brånemark. Int J Prosthodont 2015. [Google Scholar]
- R Adell. Tissue integrated prostheses in clinical dentistry. Int Dent J 1985. [Google Scholar]
- RM Sullivan. J Calif Dent Assoc. J Calif Dent Assoc 2001. [Google Scholar]
- R Adell, U Lekholm, B Rockler, PI Brånemark. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981. [Google Scholar]
- MD Rohrer, CC Schubert. The cutting-grinding technique for histologic preparation of undecalcified bone and bone-anchored implants. Improvements in instrumentation and procedures. Oral Surg Oral Med Oral Pathol 1992. [Google Scholar]
- RS Jayesh, V Dhinakarsamy. Osseointegration. J Pharm Bioallied Sci 2015. [Google Scholar]
- T Albrektsson, B Chrcanovic, M Jacobsson, A Wennerberg. Osseointegration of Implants – A Biological and Clinical Overview. JSM Dent Surg 2017. [Google Scholar]
- PI Brånemark, BO Hansson, R Adell, U Breine, J Lindström, O Hallén. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl 1977. [Google Scholar]
- R Glauser, A Rée, A Lundgren, J Gottlow, CH Hämmerle, P Schärer. Immediate occlusal loading of Brånemark implants applied in various jawbone regions: a prospective, 1-year clinical study. Clin Implant Dent Relat Res 2001. [Google Scholar]
- P Engstrand, K Gröndahl, LO Ohrnell, P Nilsson, U Nannmark, PI Brånemark. Prospective follow-up study of 95 patients with edentulous mandibles treated according to the Brånemark Novum concept. Clin Implant Dent Relat Res 2003. [Google Scholar]
- PI Brånemark, B Svensson, D Van Steenberghe. Ten-year survival rates of fixed prostheses on four or six implants ad modum Brånemark in full edentulism. Clin Oral Implants Res 1995. [Google Scholar]
- PI Brånemark, P Engstrand, LO Ohrnell, K Gröndahl, P Nilsson, K Hagberg. Brånemark Novum: A New Treatment Concept for Rehabilitation of the Edentulous Mandible. Preliminary Results from a Prospective Clinical Follow-Up Study. Clin Implant Dent Relat Res 1999. [Google Scholar]
- JP Urgell, JAV Queralt. Brånemark Novum: a new alternative for rehabitation of the lower totally edentulous jaw. RCOE 2002. [Google Scholar]
- H A Popper, M J Popper, J P Popper. The Brånemark Novum protocol: description of the treatment procedure and a clinical pilot study of 11 cases. Int J Periodontics Restorative Dent 2003. [Google Scholar]
- P A Federspil. Implant-retained craniofacial prostheses for facial defects. GMS Curr Top Otorhinolaryngol Head Neck Surg 2009. [Google Scholar] [Crossref]
- PJ Schoen, GM Raghoebar, RP Van Oort, H Reintsema, BF Van Der Laan, FR Burlage. Treatment outcome of bone-anchored craniofacial prostheses after tumor surgery. Cancer 2001. [Google Scholar]
- A Tjellström. The father of Osseointegration and the godfather of the BAHA: Professor Per-Ingvar Brånemark, Göteborg Sweden has passed away in his 86th year. Eur Arch Otorhinolaryngol 2015. [Google Scholar]
- WD Polido, A Machado-Fernandez, WS Lin, T Aghaloo. Indications for zygomatic implants: a systematic review. Int J Implant Dent 2023. [Google Scholar] [Crossref]
- SG Gil, MP Diago, JB Martínez, EM Bowen. Rehabilitation of severely resorbed maxillae with zygomatic implants: an update. Med Oral Patol Oral Cir Bucal 2007. [Google Scholar]
- Introduction
- Early life and education
- The accidental discovery of osseointegration
- Challenges in proving osseointegration
- Discussion
- Development of modern dental implantology
- Overcoming skepticism in implantology
- Pioneering osseointegration research
- Collaboration and global impact
- Other applications of osseointegration in dentistry
- Expanding applications of osseointegration
- Implant supported maxillofacial prosthesis
- Legacy and honors
- Impact on patient care
- Research and future directions
- Personal reflections and humanitarian efforts
- Conclusion
- Source of Funding
- Conflict of Interest
