- Received November 30, -0001
- Accepted November 30, -0001
- Publication June 11, 2020
- Visibility 5 Views
- Downloads 0 Downloads
- DOI 10.18231/j.aprd.2020.014
-
CrossMark
- Citation
Denture base reinforcing materials - A review
- Author Details:
-
N Prajwala *
-
C Ravi Kumar
-
M Sujesh
-
D Chalapathi Rao
-
L Pavani
Introduction
Biomaterials research has progressed steadily in the past few decades and is leading to an improvement in human life expectancy. Dental work includes changing existing materials or designing new and improved products for prosthetic applications. Dentures made of PMMA were popular because of their ability to be molded with ease, excellent esthetics and satisfactory mechanical properties. An ideal denture base material is the one that possesses biocompatibility, excellent esthetics, superior mechanical properties especially modulus of elasticity, impact strength, flexural strength and hardness, sufficient bond strength with artificial teeth, ability to repair and dimensional accuracy. [1][2]
Poly methyl methacrylate is as yet the most overwhelmingly utilized denture, but, it has certain drawbacks like thermal shrinkage, poor mechanical and fatigue strength, brittle on impact, poor color stability of self-cured resins, residual monomer allergy, porosity, poor conductors of heat and requirement of mechanical retention.[3][4] Plenty of research literature is available on denture base resins and considering their inherent drawbacks, several researches have been conducted to improve their physical and mechanical properties by reinforcing with various materials. So, this review article aims at compiling different materials from articles published through the years 1971 to 2017.
The use of hypoallergenic resins overcame the issues of monomer allergy. Therapeutic use of thermoplastic resins has increased. [3][4] Smith (1957) reported on glass reinforcement of PMMA by mixing discrete fibres with the dough or by lamination with glass cloth. Jennings & Wuebbenhorst (1960) reported on the reinforcement of pedodontic prosthetic appliances with stainless steel mesh, braided wire plate, a stainless steel lingual bar and stainless steel wire. Schreiber (1971), in a preliminary report on the reinforcement of PMMA with carbon fibres, discussed the use of acrylic resin composite prepegs. Bucknall (1977) discussed the addition of rubbers to PMMA. Bowman & Manley (1984) confirmed that the reinforcement of upper dentures with carbon fibre/PMMA inserts significantly reduced the number of breakages. Fraunhofer (1984) determined the effect of reinforcing autopolymerizing acrylic resin with flat braided two strand brass wire and orthodontic wire. Vallittu & Narva (1997) reported a composite that consists of glass fibres and aramid fibres reinforced in resin matrix.[5]
Classification
Denture base reinforcing materials are broadly classified into: Non-metals and Metals.
A. Non- Metals
1. Rubber reinforced PMMA2O3)- Zirconia (ZnO2)- Silica (SiO2)- Nanodiamond- Carbon- Halloysiteii. Nanofibers- Glass nanofibers- HA- Polyacrylonitrile and PMMA nanofibersB. Metals1. Metal fiber reinforced resins2. Metal insertsi. Stainless Steel wiresii. Brass wires3. Nanofillersi. Silverii. Copperiii. Titanium (TiO2)iv. Goldv. Platinumvi. Palladium
Rubber Reinforced Poly Methyl Methacrylate (PMMA
Sufficient impact strength and fracture toughness are most essential for denture base resins. One of the main drawbacks of PMMA denture bases is low fracture toughness. Many studies have been performed to evaluate the toughness and mechanisms of toughness improvement in rubber-modified acrylic polymers. [6][7] In these polymers, the resin matrix is filled with a rubbery particle which has a modulus of elasticity lower than that of the polymer matrix. Therefore the reinforced polymer will have a lower modulus compared to the unmodified polymer. The most significant advantage of this modification is an increase in toughness and ultimate elongation in comparison with the relatively brittle resin acrylic material.[8]
High Impact Resins
Rubber reinforced (butadiene-styrene polymethyl methacrylate) particles grafted to MMA for improved bond with PMMA. They have greater impact strength & fatigue properties and so, they are indicated for patients who drop their dentures repeatedly e.g. parkinsonism. Available as powder-liquid system & processing is samilar to heat-cure resins.
Fiber Reinforced Resins
Poor impact strength and poor fatigue resistance is primary issue with PMMA. A research by Johnston et al. reveals that within a few years of manufacture 68 percent dentures break. Mostly they are due to a combination of fatigue and impact. Fiber reinforcement leads to an improvement in strength.


| Type of fibers | Available as | Advantages | Disadvantages | |
| 1. | Metal fiber | Thin filaments of diameters from 1 to 80 micrometers | Use of full lengths of metal fibers gives the best reinforcement for strength. 12 | Resin becomes unesthetic and there is poor adhesion between metal & resin & metal is prone to corrosion. 12 |
| 2. | Carbon/ Graphite fiber | Chopped, continuous, woven, braided & tubular | Flexural, impact strengths are increased. Addition of these fibers prevent fatigue, strengthens the resin and is easy to handle. 20 | Unesthetic, polishing is difficult & weakens the denture. |
| 3. | Aramid fiber | Strength is increased. | Unesthetic, polishing is difficult. | |
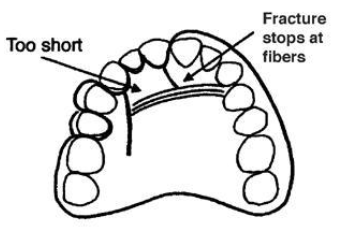
| 4. | Polyethylene fiber (Figure 1 ). | Multifibered strands | Impact strength, modulus of elasticity are improved 19 and good esthetics. | No increase in flexural strength. Placement of fibers & finishing is difficult. |
| 5. | Highly drawn linear polyethylene fibers | High tensile strength, notch insensitivity & cracks do not propagate through the fibers18 | ||
| 6. | Polypropylene fiber | Improved impact strength and highest is when treated with plasma.17 Silanized fiber improved its transverse, tensile, and impact strengths. | Wear resistance was highly decreased 17 | |
| 7. | Polyamide fiber (Nylon and Aramid) | Aramid- biocompatible, Increase in flexural strength and modulus. Nylon- increased fracture resistance and resistance to continual stress. 17 | Aramid- As fillers increased, hardness decreased. Its yellow color is a drawback. | |
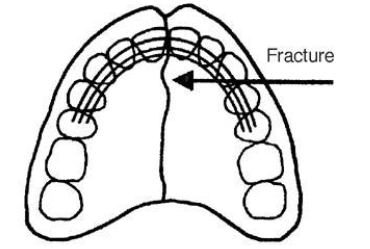
| 8. | Glass fibers (Figure 2 ). | Continuous fiber and roving, staple fiber and chopped strand mat. | Improved flexural properties and fatigue resistance. It has good aesthetics & excellent polishing characterstics. They resist extreme temperature and moisture. 16 | Void formation in fiber-polymer matrix because of poor impregnation of fibers and polymerization shrinkage. |
| 9. | E Glass fibers (Electrical grade) | Mesh and Fiber | They are transluscent thus, providing esthetics. Because of glass fiber bonding, improved strength.15 | |
| 10 | Glass nanofibers | Nanofibers | Improvements in strength, modulus, and toughness. Crack propagation is inhibited by the fibers with simultaneous reinforcement of the matrix. 14 13 | Incomplete wetting by resin, which compromises strength as the result of air inclusion and voids 27. Another drawback of nanofibers is inadequate dispersion into the resin matrix that leads to the creation of bundles. These bundles may even act as defects 26 25 |
| 11 | HA | Dispersion of HA nanofibers into a resin matrix at low mass can significantly improve the mechanical properties of the composite. 24 23 | ||
| 12 | Polyacrylonitrile (PAN) and PMMA nanofibers | PMMA is surrounded by a dental resin matrix. After curing, linear PMMA chains become interpenetrated and entangled with the cross-linked resin matrix network and produce a strong nano interface linking force with strong interfacial adhesion between nanofibers and resin matrix. 22 21 |
Position & placement of fibers
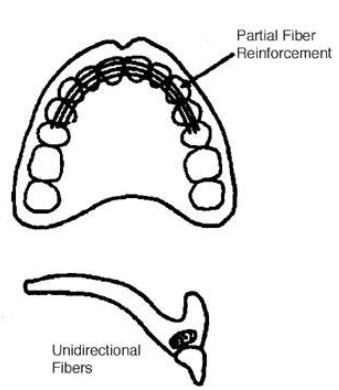
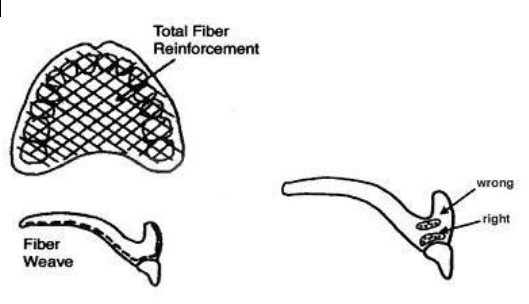
In the weak area of denture, fibers are placed [[Figure 3]]
Reinforcements are placed 90 degrees to the fracture [[Figure 4]]
Unidirectional fibers are stronger [[Figure 5]]
Mesh is to be placed on the exterior of resin surface [[Figure 6]]
Hypoallergenic Resins
Addition of hydroxyapatite fillers increases fracture toughness. [25] Addition of Al2O3 fillers increases the flexural strength & thermal diffusivity that could lead to more patient satisfaction. [26] The ratio of 2.2:1 by weight of powder to liquid was found to be the best ratio for mixing the material to give the best results in formulation. [27] [28] Addition of ceramic or sapphire whiskers to improve thermal diffusivity. [29] Addition of 11-14% of several compounds of either bismuth or uranium or 35% of an organo-zirconium compound impart radiopacity equivalent to that of aluminium. [30] Addition of Triphenyl Bismuth (Ph3Bi) is a promising new additive to provide radiopacity. [31]
Thermoplastic Resins
This new procedure, during which a fully polymerized basic material is softened by heat and injected afterwards, has opened up a new chapter in making dentures. [31]
Advantages
They provide excellent esthetics with tooth or tissue colored materials and are very comfortable for the patient. These are stable, have high fatigue endurance, high creep resistance, excellent wear characteristics & solvent resistance. They are non-porous so no growth of bacteria, and even if it is non-porous, it still retains a slight amount of moisture to keep it comfortable against gums. They are unbreakable, flexible, light weight and have very little or no monomer content. [31]
Thermoplastic nylon
The principal constituent of thermoplastic nylon is polyamide. It uses Rapid Injection which introduced the first flexite thermoplastic. Thermoplastic nylon is injected at temperatures from 274 to 293oC. This material generally replaces the metal, and the pink acrylic denture material used to build the framework for standard removable partial dentures. [32] Valplast & flexiplast are polyamides (nylon plastics), since then there is a continued interest in thermoplastic dental materials.[33], [34]
Advantages
It is virtually invisible (translucent allowing natural tissue to show through), and there are no metal clasps, only tissue coloured clasps that blend with natural teeth, thus provides excellent esthetics.[34], [35], [36], [37], [38] Nylon is unbreakable, light weight & does not warp or become brittle. Because of its flexibility & incredible patient comfort, nylon is ideal for patients considering a removable partial denture. In addition, it involves non-invasive procedures & can be relined or repaired. Nylon shows no discoloration over time & is non-porous so no growth of bacteria. [34], [35], [36], [37], [38]
Limitations
Nylon is little more difficult to trim & polish. Also it is not strong enough for conventional tooth borne rest seats. [34]
Lucitone frs flexible dental resin
Provides aesthetic partial dentures and very strong night guards when used with success injection system (closed flask system). Advantages are same as of valplast partial resin and it has more impact resistance.
Thermoplastic acetal
Acetal was first proposed as an unbreakable thermoplastic resin removable partial denture material in 1971. Rapid injection system developed the first tooth coloured clasps with thermoplastic fluoropolymer.[39] In 1986, Dental ‘D’ reintroduced tooth colored clasps using Acetal resin. Acetal as a homo-polymer has good short-term mechanical properties, but as a co-polymer has better long-term stability.
| Nanofillers | Advantages | Disadvantages | |
| 1. | Silver | They exhibit broad-spectrum bactericidal, fungicidal activities at very low concentrations and strength is increased. 44 | Discolouration of resin |
| 2. | Copper | Improved antibacterial, anti fungal properties of resin. Increased tensile and flexural strength when added in minimal concentrations | Discolouration of resin |
| 3. | TiO2 | Pleasing color, high biocompatibility, excellent mechanical properties, low cost, high stability, and appropriate antimicrobial effects 43. Has great oxidizing power under UV radiation, and can decompose organic materials and bacteria 50- 51 | |
| 4. | Alumina (Al2O3) | Improved thermal properties, flexural, tensile, compressive, impact strengths, and surface hardness of PMMA and decreased warpage. 17 | |
| 5. | Zirconia | Impact, flexural, compressive strengths have improved. Thermal conductivity fatigue strength, fracture toughness and hardness have increased. It also may have antifungal property. 17 | Occasionally, low flexural strength values have been reported. |
| 6. | Gold (Au) | Almost doubles the flexural and thermal properties, which could lead to more patient acceptance. | |
| 7. | Platinum (Pt) | Enhances mechanical properties and provides antimicrobial properties. Its addition also increases the bending deflection of denture base resin. | |
| 8. | Palladium (Pd) | Better bending strength than Gold and Silver. 17 | |
| 9. | Silicon Dioxide (SiO2) | The mechanical properties and thermal properties of PMMA were improved. Impact strength, transverse strength and surface hardness were increased. | Excess amount lead to agglomeration and crack propagation, which results in reduced hardness and fracture toughness. 17 |
| 10 | Nano diamonds | High hardness and thermal conductivity. Nano Diamonds increased the impact strength of PMMA, and also increased fracture toughness was seen. | There is agglomeration of the nanodiamonds, which may be points of stress concentration.17 |
| 11 | Copper nanotubes | CNTs are strong, resilient, and lightweight. They have excellent mechanical and electrical properties49 | The reinforcing effect of CNTs may be restricted because of weak interfacial adhesion with the resin matrix as well as the tendency of nanotubes for agglomeration, which causes poor distribution throughout the matrix. 45,46,47,48 |
Mechanism of action
Resin clasps engage the first third (or origin) of the undercut rather than the terminal third as in metal clasps allowing three to four times the retention of metal. The clasp can then be placed more gingival increasing its aesthetic appeal beyond the obvious colored properties.42
Adavntages
Thermoplastic acetal comes in 18 Vita shades + 3 pink shades, to match most people’s teeth or gums and clasps are tooth coloured clasps so provide good esthetics. Labial bars can replace bulky, un-aesthetic metal swing-lock type bars. Acetal is flexible and hypoallergenic (monomer free). The teeth and clasps can be injected together in resin, or into the existing denture adding many new applications. Adjusting is usually not necessary. [39]
Limitations
An injected resin major connector for temporary partials is no longer recommended because the major connectors must be rigid while resin is flexible and moreover it will not seal around the base of denture teeth allowing seepage of fluid under and around the teeth. Their use is limited in resin anterior teeth because it does not have the natural translucency. [39]
Applications
Acetal resin is very strong, resists wear and fracturing, and is quite flexible. These characteristics make it an ideal material for pre-formed clasps for partial dentures, single pressed unilateral partial dentures, partial denture frameworks, provisional bridges, occlusal splints, and even implant abutments.[49]
Thermoplastic acrylic
Heat-cure PMMA shows high water absorption, volumetric changes and residual monomer and porosity.[50] Even though Thermoplastic acrylic has poor impact resistance, it has enough tensile and flexural strength. It is available in tooth and gingival colors and has good esthetics. Acrylic doesn't wear as much during occlusal forces and consequently won't maintain vertical dimension over long periods of your time. [50]
Thermoplastic polycarbonate
It is a polymer chain of bisphenol-A carbonate. It is similar to Acetal resin, and is also strong, resists fracture, is flexible and does not wear. Polycarbonate is used for temporary crown & bridges. The material has a good translucency and finishes very well, providing improved esthetics. [39], [49], [50]
Advantages
It doesn’t use monomer and a catalyst in process so residual monomer doesn’t begin to melt. It also has lesser water sorption property and so, no offensive odour and does not cause redness of oral mucous membrane. [39], [49], [50]
Disadvantages
Complicated processing equipments with greater distortion from water sorption, high flexibility, low adhesion to acrylic teeth and low hardness.
Applications of thermoplastic resins
Applications of thermoplastic resins include:
Implant abutments
Preformed partial denture clasp,
Flexible tooth born partial denture framework,
Occlusal appliances,
Orthodontic and sleep apnea appliances.
Provisional crowns and bridges,
Single cast partial dentures [51]
Nanomaterials
The concept of nanotechnology was first introduced in 1959 by Feynman. Since then, nanotechnology has been widely used in many applications, including medical sciences, and plays an important role in diagnosis, treatment, and regenerative medicine.[52] A nanomaterial is an object, which at least one of its dimensions is at the nanometer scale (approximately 1 to 100 nm). Nanomaterials are categorized according to dimension – those with all 3 dimensions less than 100 nm [nanoparticles (Nps)]; those that have 2 dimensions less than 100 nm (nanotubes, nanofibers, and nanowires); and those that have one dimension less than 100 nm (thin films, layers, and coatings).[53] Use of nanomaterials in composites have achieved better esthetics and mechanical properties. [54]
Nanofillers
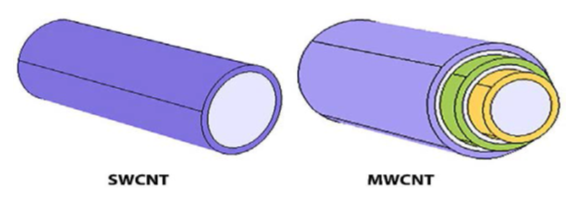
Size, shape, surface area, concentration, and dispersion of nanofillers into resin matrix all affect its mechanical properties. Alumina NPs, zirconia (ZrO2) NPs, titania (TiO2) NPs, silver NPs, gold NPs, Pt NPs, HA NPs, SiO2 NPs etc are introduced to improve the mechanical properties of PMMA. [13] Nanofillers are available in different shapes such as cones, spheres, rods, tubes and flowers. Carbon nanotubes (CNTs), ZrO2 nanotubes, TiO2 nanotubes, and halloysite nanotubes (HNT) are among the nanotubes used for reinforcement of dental materials. CNTs are classified into 2 main types according to the structure of the CNTs– single-walled and multi-walled ([Figure 7]).[55]
Self Reinforcement
Self-reinforced materials have been used in polyglycolic acid resorbable screws and plates and collagen forming materials. Gilbert, Ney & Lautenschlager in 1995, has discussed this concept of self-reinforcement of polymers. The concept is based on the idea of a fibrous material, which is chemically identical to the matrix holding the fibres in place. The composite material consisted of high strength, high ductility PMMA fibres embedded in a matrix of PMMA. The properties of unidirectional continuous form were evaluated and showed significantly greater tensile properties, flexural ductility, fracture toughness and fatigue strength compared with bulk PMMA. [5]
Conclusion
The progress in denture base resins have provided encouraging results pertaining to its strength and esthetics. Many drawbacks of PMMA denture base resins have been conqured and it is certain that in future, research will offer newer materials which are more biocompatible with better mechanical endurance, offering better treatment and care to the patient.
Source of Funding
None.
Conflict of Interest
None.
References
- Gülay Uzun, Nur Hersek, Teoman Tinçer. Effect of five woven fiber reinforcements on the impact and transverse strength of a denture base resin. J Prosth Dent 1999. [Google Scholar]
- M. Cadek, J. N. Coleman, V. Barron, K. Hedicke, W. J. Blau. Morphological and mechanical properties of carbon-nanotube-reinforced semicrystalline and amorphous polymer composites. Applied Physics Letters 2002. [Google Scholar]
- Peter Pfeiffer. the residual methyl methacrylate monomer, water sorption, and water solubility of hypoallergenic denture base materials. J Prosthet Dent 2004. [Google Scholar]
- Thomas R. Meng, Mark A. Latta. Physical Properties of Four Acrylic Denture Base Resisns. J Contemp Dent Pract 2005. [Google Scholar]
- R K Alla, S Sajjan, V R Alluri, K Ginjupalli, N Upadhya. Influence of Fiber Reinforcement on the Properties of Denture Base Resins. J Biomater Nanobiotechnol 2013. [Google Scholar]
- Zofia Danilewicz-Stysiak. Allergy as a cause of denture sore mouth. J Prosth Dent 1971. [Google Scholar]
- Shikha Nandal, Pankaj Ghalaut, Himanshu Shekhawat, Manmeet Gulati. New Era in Denture Base Resins: A Review. Dent J Adv Stud 2013. [Google Scholar]
- D. C. Jagger, A. Harrison, K. D. Jandt. The reinforcement of dentures. J Oral Rehabil 1999. [Google Scholar]
- R. Rodford. The development of high impact strength denture-base materials. J Dent 1986. [Google Scholar]
- R.A. Rodford. Further development and evaluation of high impact strength denture base materials. J Dent 1990. [Google Scholar]
- L J. Broutman, G. Panizza. Micromechanics Studies of Rubber-reinforced Glassy Polymers. Int J Polym Mater 1971. [Google Scholar]
- I E Kostoulas, V T Kavoura, M J Frangou, G L Polyzois. The effect of length parameter on the repair strength of acrylic resin using fibers or metal wires. Gen Dent 2008. [Google Scholar]
- Y Gao, S Sagi, L Zhang. Electrospun nanoscaled glass fiber reinforcement of bis-GMA/ TEGDMA dental composites. J Appl Polym Sci 2008. [Google Scholar]
- X Li, W Liu, L Sun. Resin composites reinforced by nanoscaled fibers or tubes for dental regeneration. Biomed Res Int 2014. [Google Scholar]
- Ozgul Karacaer. The effect of length & concentrationof glass fibers on the mechanical properties of an injection & a compression molded denture base polymer. J Prosthet Dent 2003. [Google Scholar]
- N.H. Ladizesky, C.F. Ho, T.W. Chow. Reinforcement of complete denture bases with continuous high performance polyethylene fibers. J Prosthet Dent 1992. [Google Scholar]
- Mohammed Gad, Shaimaa Fouda, Fahad Al-Harbi, Ritva Näpänkangas, Aune Raustia. PMMA denture base material enhancement: a review of fiber, filler, and nanofiller addition. Int J Nanomed 2017. [Google Scholar]
- Donna L. Dixon, Larry C. Breeding. The transverse strengths of three denture base resins reinforced with polyethylene fibers. J Prosthet Dent 1992. [Google Scholar]
- Susanna Segerstrom. Carbon-Graphite fiber reinforced polymers for implant superstructures. Dent Mater 2007. [Google Scholar]
- J. DeBoer, S.G. Vermilyea, R.E. Brady. The effect of carbon fiber orientation on the fatigue resistance and bending properties of two denture resins. J Prosthet Dent 1984. [Google Scholar]
- Hugo A. Vidotti, Adriana P. Manso, Victor Leung, Accácio L. do Valle, Frank Ko, Ricardo M. Carvalho. Flexural properties of experimental nanofiber reinforced composite are affected by resin composition and nanofiber/resin ratio. Dent Mater 2015. [Google Scholar]
- L Cheng, X Zhou, H Zhong. NaFloaded core-shell PAN-PMMA nanofibers as reinforcements for Bis-GMA/TEGDMA restorative resins. Mater Sci Eng C Mater Biol Appl 2013. [Google Scholar]
- Andrei Tiberiu Cucuruz, Ecaterina Andronescu, Anton Ficai, Andreia Ilie, Florin Iordache. Synthesis and characterization of new composite materials based on poly(methacrylic acid) and hydroxyapatite with applications in dentistry. Int J Pharm 2016. [Google Scholar]
- R W Arcis, A Lopez-Macipe, M Toledano. Mechanical properties of visible light-cured resins reinforced with hydroxyapatite for dental restoration. Dent Mater 2002. [Google Scholar]
- H Fong. Electrospun nylon 6 nanofiber reinforced BIS-GMA/TEGDMA dental restorative composite resins. Polymer 2004. [Google Scholar]
- L Chen, C Xu, Y Wang. BisGMA/TEGDMA dental nanocomposites containing glyoxylic acid-modified high-aspect ratio hydroxyapatite nanofibers with enhanced dispersion. Biomed Mater 2012. [Google Scholar]
- Stephen A. Boyd, Bo Su, Jonathan R. Sandy, Anthony J. Ireland. Cellulose Nanofibre Mesh for Use in Dental Materials. Coatings 2012. [Google Scholar]
- Peter Pfeiffer, Ernst-Ulrich Rosenbauer. Residual methyl methacrylate monomer, water sorption, and water solubility of hypoallergenic denture base materials. J Prosthet Dent 2004. [Google Scholar]
- Naomi Tanoue, Kiyoshi Nagano, Hideo Matsumura. Use of a light-polymerized composite removable partial denture base for a patient hypersensitive to poly(methyl methacrylate), polysulfone, and polycarbonate: A clinical report. J Prosthet Dent 2005. [Google Scholar]
- S H Mohamed, A Arifin, Z A Mohd Ishak, A Nizam, A R Samsudin. Mechanical & thermal properties of hydroxyapatite filled poly (methyl methacrylate) heat processed denture base material. Med J Malaysia 2004. [Google Scholar]
- A E Ellakwa. The effect of aluminium oxide on the Flexural Strength and Thermal Diffusivity of Heat Polymerized acrylic resin. J Prosthod 2008. [Google Scholar]
- S H Mohamed, A Arifin, Mohd Ishak, Z A Nizam, A Samsudin, A R. The Effect Of Powder To Liquid Ratio On Tensile Strength And Glass Transition Temperature Of Alumina Filled Poly Methyl Methacrylate (PMMA) Denture Base Material. Med J Malaysia 2004. [Google Scholar]
- C Pesci Bardon, T Fosse, D Serre, I Medenier. Effect Of 2% quaternary ammonium compound polymerised with a denture acrylic resin. Gerodontology 2006. [Google Scholar]
- Philip B. The New Acrylic Resin With Improved Thermal Diffusivity. J Prosthet Dent 1998. [Google Scholar]
- H.R. Rawls, J. Starr, F.H. Kasten, M. Murray, J. Smid, I. Cabasso. Radiopaque acrylic resins containing miscible heavy-metal compounds. Dent Mater 1990. [Google Scholar]
- H.R. Rawls, M.V. Marshall, H.L. Cardenas, H.R. Bhagat, I. Cabasso. Cytotoxicity evaluation of a new radiopaque resin additive—triphenyl bismuth. Dent Mater 1992. [Google Scholar]
- M Negruţiu, C Sinescu, Sandu Liliana. . Guidelines of removable partial dentures 2004. [Google Scholar]
- L G Lowe. Flexible denture flanges for patients exhibiting undercut tuberosities and reduced width of the buccal vestibule: a clinical report. J Prosthet Dent 2004. [Google Scholar]
- Rodney D. Phoenix, Michael A. Mansueto, Neal A. Ackerman, Robert E. Jones. Evaluation of Mechanical and Thermal Properties of Commonly Used Denture Base Resins. J Prosthodont 2004. [Google Scholar]
- R Janda. Prothesenkunststoffe aus werkstoffkundlicher Sicht. Quintessenz Zahntech 1997. [Google Scholar]
- M Negruţiu, M Romînu, Z Floriţa. Influenţa tehnologiei de prelucrare asupra calităţii polimerilor pentru proteze mobile şi mobilizabile. Revista de Stomatologie 2001. [Google Scholar]
- Ali Parvizi, Terry Lindquist, Robert Schneider, Derrick Williamson, Daniel Boyer, Deborah V. Dawson. Comparison of the Dimensional Accuracy of Injection‐Molded Denture Base Materials to that of Conventional Pressure‐Pack Acrylic Resin. J Prosthodont 2004. [Google Scholar]
- A Chatterjee. Properties improvement of PMMA using nano TiO2. J Appl Polym Sci 2010. [Google Scholar]
- Indumathi Sivakumar, Kuthalingam Subbiah Arunachalam, Suresh Sajjan, Alluri Venkata Ramaraju, Bheemalingeshwara Rao, Bindu Kamaraj. Incorporation of Antimicrobial Macromolecules in Acrylic Denture Base Resins: A Research Composition and Update. J Prosthodont 2014. [Google Scholar]
- Xiaoming Li, Yubo Fan, Fumio Watari. Current investigations into carbon nanotubes for biomedical application. Biomedical Materials 2010. [Google Scholar] [Crossref]
- Hamouda. Current perspectives of nanoparticles in medical and dental biomaterials. Journal of Biomedical Research 2012. [Google Scholar] [Crossref]
- J Chen, A M Rao, S Lyuksyutov. Dissolution of full-length single-walled carbon nanotubes. J Phys Chem B 2001. [Google Scholar]
- F Zhang, Y Xia, L Xu. Surface modification and microstructure of single-walled carbon nanotubes for dental resin-based composites. J Biomed Mater Res B Appl Biomater 2008. [Google Scholar]
- R Wang, J Tao, B Yu. Characterization of multiwalled carbon nanotube-polymethyl methacrylate composite resins as denture base materials. J Prosthet Dent 2014. [Google Scholar]
- Shaymaa E. Elsaka, Ibrahim M. Hamouda, Michael V. Swain. Titanium dioxide nanoparticles addition to a conventional glass-ionomer restorative: Influence on physical and antibacterial properties. J Dent 2011. [Google Scholar]
- Sama A. Alwan, Shatha S. Alameer. The Effect of the Addition of Silanized Nano Titania Fillers on Some Physical and Mechanical Properties of Heat Cured Acrylic Denture Base Materials. J Baghdad Coll Dent 2015. [Google Scholar]
- Phillip L.J. Keenan, David R. Radford, Robert K.F. Clark. Dimensional change in complete dentures fabricated by injection molding and microwave processing. J Prosthet Dent 2003. [Google Scholar]
- T E Donovan, G C Cho. Esthetic considerations with removable partial dentures. J Calif Dent Assoc 2003. [Google Scholar]
- Meda Negrutiu, Cosmin Sinescu, Mihai Romanu, Daniela Pop, Sorin Lakatos. Thermoplastic Resins for Flexible Framework Removable Partial Dentures. TMJ 2005. [Google Scholar]
- R Janda. Prothesenkunststoffe aus werkstoffkundlicher Sicht. Quintessenz Zahntech 1997. [Google Scholar]
- A M Grumezescu. Nanobiomaterials in Dentistry Applications of Nanobiomaterials. 2016. [Google Scholar]
- Luisa F, Duncan S European Commission. Nanotechnologies: Principles, Applications, Implications and Hands-on Activities.. 2012. [Google Scholar]
- S Hoshika, F Nagano, T Tanaka. Expansion of nanotechnology for dentistry: effect of colloidal platinum nanoparticles on dentin adhesion mediated by 4-META/MMA-TBB. J Adhes Dent 2011. [Google Scholar]
